
Back علاج السل Arabic Tractament de la tuberculosi Catalan तपेदिक उपचार Hindi 結核の管理 Japanese 결핵의 치료 Korean Tuberculostático Portuguese Лечение туберкулёза Russian Tuberculosis treatment SIMPLE క్షయవ్యాధి చికిత్స Tegulu Quản lý bệnh lao Vietnamese
| Management of tuberculosis | |
|---|---|
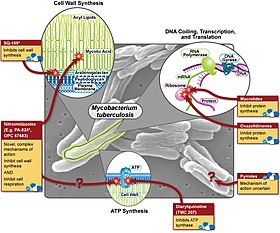 Various pharmaceutical tuberculosis treatments and their actions | |
| Specialty | Infectious diseases |
Management of tuberculosis refers to techniques and procedures utilized for treating tuberculosis (TB), or simply a treatment plan for TB.
The medical standard for active TB is a short course treatment involving a combination of isoniazid, rifampicin (also known as Rifampin), pyrazinamide, and ethambutol for the first two months. During this initial period, Isoniazid is taken alongside pyridoxal phosphate to obviate peripheral neuropathy. Isoniazid is then taken concurrently with rifampicin for the remaining four months of treatment (6-8 months for Miliary tuberculosis). A patient is expected to be free from all living TB bacteria after six months of therapy in Pulmonary TB or 8-10 months in Miliary TB.[citation needed]
Latent tuberculosis or latent tuberculosis infection (LTBI) is treated with three to nine months of isoniazid alone. This long-term treatment often risks the development of hepatotoxicity. A combination of isoniazid plus rifampicin for a period of three to four months is shown to be an equally effective method for treating LTBI, while mitigating risks to hepatotoxicity. Treatment of LTBI is essential in preventing the spread of active TB.[1][2][3]
- ^ Sterling TR, Villarino ME, Borisov AS, Shang N, Gordin F, Bliven-Sizemore E, et al. (December 2011). "Three months of rifapentine and isoniazid for latent tuberculosis infection". The New England Journal of Medicine. 365 (23): 2155–66. doi:10.1056/nejmoa1104875. PMID 22150035.
- ^ World Health Organization (2014). Guidelines on the management of latent tuberculosis infection. World Health Organization (WHO). hdl:10665/136471. ISBN 978-92-4-154890-8. WHO/HTM/TB/2015.01. Archived from the original on 5 June 2015.
- ^ World Health Organization (2015). Evidence to decision framework: appendix to the guidelines on the management of latent tuberculosis infection. World Health Organization (WHO). hdl:10665/158915. WHO/HTM/TB/2015.01.