
Back Antikörper ALS ኣንቲቦዲ Amharic جسم مضاد Arabic প্ৰতিদেহ Assamese Antitel Azerbaijani Антыцелы Byelorussian Антитяло Bulgarian प्रतीदेह Bihari অ্যান্টিবডি Bengali/Bangla Antitijelo BS
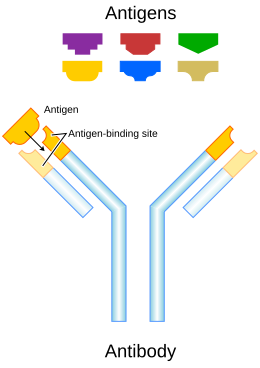
An antibody (Ab) is the secreted form of a B cell receptor; the term immunoglobulin (Ig) can refer to either the membrane-bound form or the secreted form of the B cell receptor, but they are, broadly speaking, the same protein, and so the terms are often treated as synonymous.[1] Antibodies are large, Y-shaped proteins belonging to the immunoglobulin superfamily which are used by the immune system to identify and neutralize foreign objects such as bacteria and viruses, including those that cause disease. Antibodies can recognize virtually any size antigen with diverse chemical compositions from molecules.[2] Each antibody recognizes one or more specific antigens.[3][4] This term literally means "antibody generator", as it is the presence of an antigen that drives the formation of an antigen-specific antibody. Each tip of the "Y" of an antibody contains a paratope that specifically binds to one particular epitope on an antigen, allowing the two molecules to bind together with precision. Using this mechanism, antibodies can effectively "tag" a microbe or an infected cell for attack by other parts of the immune system, or can neutralize it directly (for example, by blocking a part of a virus that is essential for its invasion).
To allow the immune system to recognize millions of different antigens, the antigen-binding sites at both tips of the antibody come in an equally wide variety. The rest of the antibody structure is relatively generic. In humans, antibodies occur in five classes, sometimes called isotypes: IgA, IgD, IgE, IgG, and IgM. Human IgG and IgA antibodies are also divided into discrete subclasses (IgG1, IgG2, IgG3, IgG4; IgA1 and IgA2). The class refers to the functions triggered by the antibody (also known as effector functions), in addition to some other structural features. Antibodies from different classes also differ in where they are released in the body and at what stage of an immune response. Importantly, while classes and subclasses of antibodies may be shared between species (at least in name), their functions and distribution throughout the body may be different. For example, mouse IgG1 is closer to human IgG2 than human IgG1 in terms of its function.
The term humoral immunity is often treated as synonymous with the antibody response, describing the function of the immune system that exists in the body's humors (fluids) in the form of soluble proteins, as distinct from cell-mediated immunity, which generally describes the responses of T cells (especially cytotoxic T cells). In general, antibodies are considered part of the adaptive immune system, though this classification can become complicated. For example, natural IgM,[5] which are made by B-1 lineage cells that have properties more similar to innate immune cells than adaptive, refers to IgM antibodies made independently of an immune response that demonstrate polyreactivity- they recognize multiple distinct (unrelated) antigens. These can work with the complement system in the earliest phases of an immune response to help facilitate clearance of the offending antigen and delivery of the resulting immune complexes to the lymph nodes or spleen for initiation of an immune response. Hence in this capacity, the function of antibodies is more akin to that of innate immunity than adaptive. Nonetheless, in general antibodies are regarded as part of the adaptive immune system because they demonstrate exceptional specificity (with some exception), are produced through genetic rearrangements (rather than being encoded directly in germline), and are a manifestation of immunological memory.
In the course of an immune response, B cells can progressively differentiate into antibody-secreting cells (B cells themselves do not secrete antibody; B cells do, however, express B cell receptors, the membrane-bound form of the antibody, on their surface) or memory B cells.[6] Antibody-secreting cells comprise plasmablasts and plasma cells, which differ mainly in the degree to which they secrete antibody, their lifespan, metabolic adaptations, and surface markers.[7] Plasmablasts are rapidly proliferating, short-lived cells produced in the early phases of the immune response (classically described as arising extrafollicularly rather than from the germinal center) which have the potential to differentiate further into plasma cells.[8] The literature is sloppy at times and often describes plasmablasts as just short-lived plasma cells- formally this is incorrect. Plasma cells, in contrast, do not divide (they are terminally differentiated), and rely on survival niches comprising specific cell types and cytokines to persist.[9] Plasma cells will secrete huge quantities of antibody regardless of whether or not their cognate antigen is present, ensuring that antibody levels to the antigen in question do not fall to 0, provided the plasma cell stays alive. The rate of antibody secretion, however, can be regulated, for example, by the presence of adjuvant molecules that stimulate the immune response such as TLR ligands.[10] Long-lived plasma cells can live for potentially the entire lifetime of the organism.[11] Classically, the survival niches that house long-lived plasma cells reside in the bone marrow,[12] though it cannot be assumed that any given plasma cell in the bone marrow will be long-lived. However, other work indicates that survival niches can readily be established within the mucosal tissues- though the classes of antibodies involved show a different hierarchy from those in the bone marrow.[13][14] B cells can also differentiate into memory B cells which can persist for decades similarly to long-lived plasma cells. These cells can be rapidly recalled in a secondary immune response, undergoing class switching, affinity maturation, and differentiating into antibody-secreting cells.
Antibodies are central to the immune protection elicited by most vaccines and infections (although other components of the immune system certainly participate and for some diseases are considerably more important than antibodies in generating an immune response, e.g. herpes zoster).[15] Durable protection from infections caused by a given microbe – that is, the ability of the microbe to enter the body and begin to replicate (not necessarily to cause disease) – depends on sustained production of large quantities of antibodies, meaning that effective vaccines ideally elicit persistent high levels of antibody, which relies on long-lived plasma cells. At the same time, many microbes of medical importance have the ability to mutate to escape antibodies elicited by prior infections, and long-lived plasma cells cannot undergo affinity maturation or class switching. This is compensated for through memory B cells: novel variants of a microbe that still retain structural features of previously encountered antigens can elicit memory B cell responses that adapt to those changes. It has been suggested that long-lived plasma cells secrete B cell receptors with higher affinity than those on the surfaces of memory B cells, but findings are not entirely consistent on this point.[16]
- ^ Rhoades RA, Pflanzer RG (2002). Human Physiology (5th ed.). Thomson Learning. p. 584. ISBN 978-0-534-42174-8.
- ^ Wilson IA, Stanfield RL (3 May 2021). "50 Years of structural immunology". The Journal of Biological Chemistry. 296: 100745. doi:10.1016/j.jbc.2021.100745. ISSN 0021-9258. PMC 8163984. PMID 33957119.
Antibodies (A–D) can recognize virtually any antigen whether large or small, and which can have diverse chemical compositions from small molecules (A) to carbohydrates to lipids to peptides (B) to proteins (C and D) and combinations thereof.
- ^ Janeway C (2001). Immunobiology (5th ed.). Garland Publishing. ISBN 978-0-8153-3642-6.
- ^ Litman GW, Rast JP, Shamblott MJ, Haire RN, Hulst M, Roess W, et al. (January 1993). "Phylogenetic diversification of immunoglobulin genes and the antibody repertoire". Molecular Biology and Evolution. 10 (1): 60–72. doi:10.1093/oxfordjournals.molbev.a040000. PMID 8450761.
- ^ Ehrenstein MR, Notley CA (15 October 2010). "The importance of natural IgM: scavenger, protector and regulator". Nature Reviews Immunology. 10 (11): 778–786. doi:10.1038/nri2849. ISSN 1474-1733. PMID 20948548. S2CID 35784099.
- ^ Akkaya M, Kwak K, Pierce SK (April 2020). "B cell memory: building two walls of protection against pathogens". Nature Reviews Immunology. 20 (4): 229–238. doi:10.1038/s41577-019-0244-2. ISSN 1474-1741. PMC 7223087. PMID 31836872.
- ^ Tellier J, Nutt SL (15 October 2018). "Plasma cells: The programming of an antibody-secreting machine". European Journal of Immunology. 49 (1): 30–37. doi:10.1002/eji.201847517. hdl:11343/284565. ISSN 0014-2980. PMID 30273443.
- ^ "B Cell Memory and Plasma Cell Development", Molecular Biology of B Cells, Elsevier, pp. 227–249, 2015, doi:10.1016/b978-0-12-397933-9.00014-x, ISBN 978-0-12-397933-9, retrieved 24 January 2024
- ^ Chu VT, Berek C (19 December 2012). "The establishment of the plasma cell survival niche in the bone marrow". Immunological Reviews. 251 (1): 177–188. doi:10.1111/imr.12011. ISSN 0105-2896. PMID 23278749. S2CID 205212187.
- ^ Dorner M, Brandt S, Tinguely M, Zucol F, Bourquin JP, Zauner L, et al. (6 November 2009). "Plasma cell toll-like receptor (TLR) expression differs from that of B cells, and plasma cell TLR triggering enhances immunoglobulin production". Immunology. 128 (4): 573–579. doi:10.1111/j.1365-2567.2009.03143.x. ISSN 0019-2805. PMC 2792141. PMID 19950420.
- ^ Joyner CJ, Ley AM, Nguyen DC, Ali M, Corrado A, Tipton C, et al. (March 2022). "Generation of human long-lived plasma cells by developmentally regulated epigenetic imprinting". Life Science Alliance. 5 (3): e202101285. doi:10.26508/lsa.202101285. ISSN 2575-1077. PMC 8739272. PMID 34952892.
- ^ Halliley JL, Tipton CM, Liesveld J, Rosenberg AF, Darce J, Gregoretti IV, et al. (July 2015). "Long-Lived Plasma Cells Are Contained within the CD19−CD38hiCD138+ Subset in Human Bone Marrow". Immunity. 43 (1): 132–145. doi:10.1016/j.immuni.2015.06.016. PMC 4680845. PMID 26187412.
- ^ Tellier J, Tarasova I, Nie J, Smillie CS, Fedele PL, Cao WH, et al. (3 January 2024). "Unraveling the diversity and functions of tissue-resident plasma cells". Nature Immunology. 25 (2): 330–342. doi:10.1038/s41590-023-01712-w. ISSN 1529-2908. PMID 38172260. S2CID 266752931.
- ^ Landsverk OJ, Snir O, Casado RB, Richter L, Mold JE, Réu P, et al. (February 2017). "Antibody-secreting plasma cells persist for decades in human intestine". The Journal of Experimental Medicine. 214 (2): 309–317. doi:10.1084/jem.20161590. ISSN 1540-9538. PMC 5294861. PMID 28104812.
- ^ Plotkin SA (2022). "Recent updates on correlates of vaccine-induced protection". Frontiers in Immunology. 13: 1081107. doi:10.3389/fimmu.2022.1081107. ISSN 1664-3224. PMC 9912984. PMID 36776392.
- ^ Sutton HJ, Gao X, Kelly HG, Parker BJ, Lofgren M, Dacon C, et al. (12 January 2024). "Lack of affinity signature for germinal center cells that have initiated plasma cell differentiation". Immunity. 57 (2): S1074–7613(23)00541–1. doi:10.1016/j.immuni.2023.12.010. ISSN 1097-4180. PMC 10922795. PMID 38228150.