Back بوابة:علم الفيروسات Arabic درگاه:ویروس Persian Portail:Virologie French Portal:Virus ID Portal:Vírus Portuguese ද්වාරය:වෛරස Singhalese باب:وائرسز Urdu Portal:病毒 Chinese
The Viruses Portal
Welcome!
Viruses are small infectious agents that can replicate only inside the living cells of an organism. Viruses infect all forms of life, including animals, plants, fungi, bacteria and archaea. They are found in almost every ecosystem on Earth and are the most abundant type of biological entity, with millions of different types, although only about 6,000 viruses have been described in detail. Some viruses cause disease in humans, and others are responsible for economically important diseases of livestock and crops.
Virus particles (known as virions) consist of genetic material, which can be either DNA or RNA, wrapped in a protein coat called the capsid; some viruses also have an outer lipid envelope. The capsid can take simple helical or icosahedral forms, or more complex structures. The average virus is about 1/100 the size of the average bacterium, and most are too small to be seen directly with an optical microscope.
The origins of viruses are unclear: some may have evolved from plasmids, others from bacteria. Viruses are sometimes considered to be a life form, because they carry genetic material, reproduce and evolve through natural selection. However they lack key characteristics (such as cell structure) that are generally considered necessary to count as life. Because they possess some but not all such qualities, viruses have been described as "organisms at the edge of life".
Selected disease
Rabies is a disease of humans and some other mammals, generally caused by the rabies virus, an RNA virus in the Rhabdoviridae family. A few cases have involved the closely related Australian bat lyssavirus. Rabies virus has a wide host range. Globally, dogs are the main source of human infections, with bats being important in the Americas; other naturally infected animals include monkeys, raccoons, foxes, skunks, cattle, horses, wolves, coyotes, cats, mongooses, bears, groundhogs, weasels and other carnivores. Transmission is commonly via saliva, usually but not always from bites; it can potentially occur via aerosols contacting mucous membranes. The typical human incubation period is 1–3 months. The neurotropic virus travels along neural pathways into the CNS and brain, where it causes meningoencephalitis. Nonspecific symptoms such as fever and headache are followed by neurological symptoms, including partial paralysis, confusion, agitation, paranoia, hallucinations and sometimes hydrophobia, which progress to delirium, coma and death. Around 17,400 people died from rabies in 2015, mainly in Asia and Africa.
Rabies is mentioned in the Codex of Eshnunna of around 1930 BC. The first vaccine was developed in 1885 by Louis Pasteur and Émile Roux. Prophylactic vaccination is used in people at high risk, pets and wild animals. Post-exposure prophylaxis, including vaccine and immunoglobulin, is completely effective if begun immediately after exposure, but survival is extremely rare once symptoms have begun.
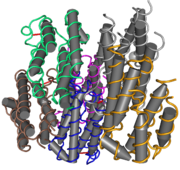
Selected image
Some viruses, such as the T7 bacteriophage, encode their own RNA polymerase, the enzyme that makes messenger RNA based on a DNA template. The T7 enzyme has a single subunit, and is more like chloroplast and mitochondrial enzymes than those of bacteria or the cell.
Credit: Thomas Splettstoesser (25 June 2007)
In the news
26 February: In the ongoing pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), more than 110 million confirmed cases, including 2.5 million deaths, have been documented globally since the outbreak began in December 2019. WHO
18 February: Seven asymptomatic cases of avian influenza A subtype H5N8, the first documented H5N8 cases in humans, are reported in Astrakhan Oblast, Russia, after more than 100,0000 hens died on a poultry farm in December. WHO
14 February: Seven cases of Ebola virus disease are reported in Gouécké, south-east Guinea. WHO
7 February: A case of Ebola virus disease is detected in North Kivu Province of the Democratic Republic of the Congo. WHO
4 February: An outbreak of Rift Valley fever is ongoing in Kenya, with 32 human cases, including 11 deaths, since the outbreak started in November. WHO
21 November: The US Food and Drug Administration (FDA) gives emergency-use authorisation to casirivimab/imdevimab, a combination monoclonal antibody (mAb) therapy for non-hospitalised people twelve years and over with mild-to-moderate COVID-19, after granting emergency-use authorisation to the single mAb bamlanivimab earlier in the month. FDA 1, 2
18 November: The outbreak of Ebola virus disease in Équateur Province, Democratic Republic of the Congo, which started in June, has been declared over; a total of 130 cases were recorded, with 55 deaths. UN
Selected article
Interferons are a group of signalling proteins released by host cells in response to viruses and other pathogens. They belong to a large class of proteins known as cytokines: molecules used for communication between cells to trigger the protective defences of the immune system that help to eradicate pathogens. More than twenty distinct interferon genes and proteins have been identified in animals, including humans.
When a cell is infected by a virus, several virus products, including glycoproteins and viral RNA, stimulate the cell to produce and release interferons. This causes nearby cells to heighten their defences against viral infection, and so interferes with viral replication. Some viruses, including Japanese encephalitis virus, dengue type 2 virus, human cytomegalovirus and Kaposi's sarcoma-associated herpesvirus, have evolved ways to resist interferon's antiviral activity. Interferons also have various other functions in regulating the immune system. Interferons and other cytokines are responsible for some symptoms of infection, such as fever, muscle pain and "flu-like symptoms".
Selected outbreak
The last recorded smallpox death occurred during the 1978 smallpox outbreak in Birmingham, UK. The outbreak resulted from accidental exposure to the Abid strain of Variola major, from a laboratory, headed by Henry Bedson, at the University of Birmingham Medical School – also associated with an outbreak in 1966. Bedson was investigating strains of smallpox known as whitepox, considered a potential threat to the smallpox eradication campaign, then in its final stages.
A medical photographer who worked on the floor above the laboratory showed smallpox symptoms in August and died the following month; one of her contacts was also infected but survived. The government inquiry into the outbreak concluded that she had been infected in late July, possibly via ducting, although the precise route of transmission was subsequently challenged. The inquiry criticised the university's safety procedures. Bedson committed suicide while under quarantine. Radical changes in UK research practices for handling dangerous pathogens followed, and all known stocks of smallpox virus were concentrated in two laboratories.
Selected quotation
| “ | A virus is not an individual organism in the ordinary sense of the term, but something which could almost be called a stream of biological patterns. | ” |
Recommended articles
Viruses & Subviral agents: bat virome • elephant endotheliotropic herpesvirus • HIV • introduction to viruses![]() • Playa de Oro virus • poliovirus • prion • rotavirus
• Playa de Oro virus • poliovirus • prion • rotavirus![]() • virus
• virus![]()
Diseases: colony collapse disorder • common cold • croup • dengue fever![]() • gastroenteritis • Guillain–Barré syndrome • hepatitis B • hepatitis C • hepatitis E • herpes simplex • HIV/AIDS • influenza
• gastroenteritis • Guillain–Barré syndrome • hepatitis B • hepatitis C • hepatitis E • herpes simplex • HIV/AIDS • influenza![]() • meningitis
• meningitis![]() • myxomatosis • polio
• myxomatosis • polio![]() • pneumonia • shingles • smallpox
• pneumonia • shingles • smallpox
Epidemiology & Interventions: 2007 Bernard Matthews H5N1 outbreak • Coalition for Epidemic Preparedness Innovations • Disease X • 2009 flu pandemic • HIV/AIDS in Malawi • polio vaccine • Spanish flu • West African Ebola virus epidemic
Virus–Host interactions: antibody • host • immune system![]() • parasitism • RNA interference
• parasitism • RNA interference![]()
Methodology: metagenomics
Social & Media: And the Band Played On • Contagion • "Flu Season" • Frank's Cock![]() • Race Against Time: Searching for Hope in AIDS-Ravaged Africa
• Race Against Time: Searching for Hope in AIDS-Ravaged Africa![]() • social history of viruses
• social history of viruses![]() • "Steve Burdick" • "The Time Is Now" • "What Lies Below"
• "Steve Burdick" • "The Time Is Now" • "What Lies Below"
People: Brownie Mary • Macfarlane Burnet![]() • Bobbi Campbell • Aniru Conteh • people with hepatitis C
• Bobbi Campbell • Aniru Conteh • people with hepatitis C![]() • HIV-positive people
• HIV-positive people![]() • Bette Korber • Henrietta Lacks • Linda Laubenstein • Barbara McClintock
• Bette Korber • Henrietta Lacks • Linda Laubenstein • Barbara McClintock![]() • poliomyelitis survivors
• poliomyelitis survivors![]() • Joseph Sonnabend • Eli Todd • Ryan White
• Joseph Sonnabend • Eli Todd • Ryan White![]()
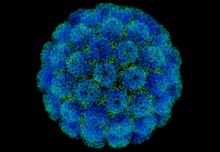
Selected virus
Acanthamoeba polyphaga mimivirus (APMV) is a species of DNA virus in the Mimivirus genus of the Mimiviridae family. It infects the amoeba, Acanthamoeba polyphaga. Its non-enveloped icosahedral capsid is 400 nm in diameter, with protein filaments of 100 nm projecting from its surface. The APMV genome is a linear, double-stranded DNA molecule of around 1.2 megabases, encoding around 979 genes. This is comparable to the genome of some small bacteria. It encodes several proteins that had not been previously discovered in viruses, including aminoacyl tRNA synthetases. APMV is itself parasitised by the Sputnik virophage (arrowed in micrograph).
APMV is as large as some small species of bacteria, such as Rickettsia conorii and Tropheryma whipplei. When it was first discovered in 1992, it was thought to be a bacterium, and named Bradfordcoccus. APMV was not shown to be a virus until 2003, when it was the largest virus then discovered. It has since been overtaken by Megavirus chilensis, Pandoravirus and Pithovirus, all of which also infect amoebae. These and other large and complex DNA viruses are now grouped in Nucleocytoviricota, also termed nucleocytoplasmic large DNA viruses.
Did you know?
- ...that the elegant rice rat (pictured; top) sometimes carries a hantavirus that can cause a fatal disease in humans?
- ...that a quaranjavirus that can infect humans was discovered in 1953, but it took 60 years to classify it?
- ...that in 1918, infected crew members aboard HMS Mantua inadvertently spread the Spanish flu to Africa?
- ...that in the mid-1980s, some HIV patients pinned their hopes for survival on an experimental drug called HPA-23?
- ...that Li Zaiping and his research group were the first to sequence a viral genome in China?
Selected biography
Peter Piot (born 17 February 1949) is a Belgian virologist and public health specialist, known for his work on Ebola virus and HIV.
During the first outbreak of Ebola in Yambuku, Zaire in 1976, Piot was one of a team that discovered the filovirus in a blood sample. He and his colleagues travelled to Zaire to help to control the outbreak, and showed that the virus is transmitted via blood and during preparation of bodies for burial. He advised WHO during the West African Ebola epidemic of 2014–16.
In the 1980s, Piot participated in collaborative projects in Burundi, Côte d'Ivoire, Kenya, Tanzania and Zaire, including Project SIDA in Kinshasa, the first international project on AIDS in Africa, which provided the foundations for understanding HIV infection in that continent. He was the founding director of UNAIDS, and has served as president of the International AIDS Society and assistant director of the WHO Global HIV/AIDS Programme. As of 2020, he directs the London School of Hygiene & Tropical Medicine.
In this month
5 June 1981: First report of HIV/AIDS (symbol pictured) appeared in medical literature
6 June 1997: Gene silencing in plants shown to be a viral defence mechanism
7–13 June 1962: Donald Caspar and Aaron Klug proposed the quasi-equivalence principle of virus structure
7–13 June 1962: André Lwoff proposed a viral classification scheme based on nature of genome, type of symmetry and presence of envelope
7–13 June 1962: George Hirst proposed that the influenza virus genome is segmented
9 June 1981: The American Society for Virology was founded
13 June 2012: First case of Middle East respiratory syndrome coronavirus (MERS-CoV) occurred in Saudi Arabia
18 June 1981: A vaccine against foot-and-mouth disease was the first genetically engineered vaccine
21 June 1996: Nevirapine approved, first NNRTI for HIV/AIDS
26 June 1993: Clinical trial of hepatitis B virus drug fialuridine terminated; the drug caused several fatalities due to lactic acidosis
28 June 2011: FAO declared rinderpest eradicated
30 June 1985: Ryan White was denied re-admittance to his school after an AIDS diagnosis, in a case that changed public perceptions of the disease
Selected intervention
Influenza vaccines include live attenuated and inactivated forms. Inactivated vaccines contain three or four different viral strains selected by the World Health Organization to cover influenza A H1N1 and H3N2, as well as influenza B, and are usually administered by intramuscular injection. The live attenuated influenza vaccine contains a cold-adapted strain and is given as a nasal spray. Most influenza vaccine strains are cultivated in fertilised chicken eggs (pictured), a technique developed in the 1950s; others are grown in cell cultures, and some vaccines contain recombinant proteins. Annual vaccination is recommended for high-risk groups and, in some countries, for all those over six months. As the influenza virus changes rapidly by antigenic drift, new versions of the vaccine are developed twice a year, which differ in effectiveness depending on how well they match the circulating strains. Despite considerable research effort for decades, no effective universal influenza vaccine has been identified. A 2018 meta-analysis found that vaccination in healthy adults decreased confirmed cases of influenza from about 2.4% to 1.1%. However, the effectiveness is uncertain in those over 65 years old, one of the groups at highest risk of serious complications.
Subcategories
Subcategories of virology:
Topics
Things to do
- Comment on what you like and dislike about this portal
- Join the Viruses WikiProject
- Tag articles on viruses and virology with the project banner by adding {{WikiProject Viruses}} to the talk page
- Assess unassessed articles against the project standards
- Create requested pages: red-linked viruses | red-linked virus genera
- Expand a virus stub into a full article, adding images, citations, references and taxoboxes, following the project guidelines
- Create a new article (or expand an old one 5-fold) and nominate it for the main page Did You Know? section
- Improve a B-class article and nominate it for Good Article
 or Featured Article
or Featured Article status
status - Suggest articles, pictures, interesting facts, events and news to be featured here on the portal
WikiProjects & Portals
 WikiProject Viruses
Related WikiProjects
WikiProject Viruses
Related WikiProjects
Medicine • Microbiology • Molecular & Cellular Biology • Veterinary Medicine
Related PortalsAssociated Wikimedia
The following Wikimedia Foundation sister projects provide more on this subject:
-
Commons
Free media repository -
Wikibooks
Free textbooks and manuals -
Wikidata
Free knowledge base -
Wikinews
Free-content news -
Wikiquote
Collection of quotations -
Wikisource
Free-content library -
Wikispecies
Directory of species -
Wikiversity
Free learning tools -
Wiktionary
Dictionary and thesaurus